Peripheral Arterial Disease reduces your quality of life
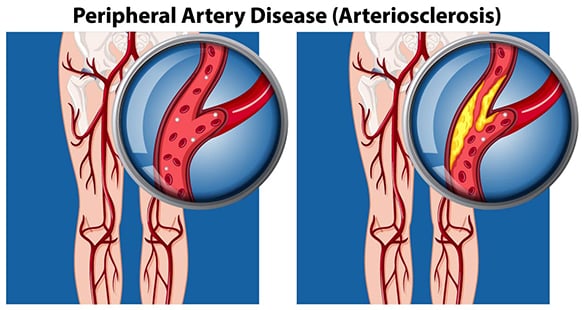
Peripheral Arterial Disease (PAD) is a circulation problem caused by a buildup of fatty deposits along the walls of your arteries, leading to insufficient blood flow to the muscles of your legs and feet. The resulting muscle pain can severely reduce your quality of life, but PAD also increases your risk of heart attack and stroke. An estimated one in three people with diabetes over the age of 50 have PAD.
How is Peripheral Arterial Disease different from Diabetic Peripheral Neuropathy?
Peripheral Arterial Disease differs from Diabetic Peripheral Neuropathy in that the latter affects the nerves, whereas PAD affects the blood vessels and circulation.
How does diabetes lead to Peripheral Arterial Disease?
Diabetes leads to the development of PAD by promoting antherosclerosis, or the narrowing of your arteries. Diabetes promotes antherosclerosis by:
- increasing the levels of two important fats, trigylcerides and cholesteroal, in your blood, which then accumulate on the walls of your arteries
- increasing your blood sugar levels, which then interfere with the structure and function of your blood vessels


How do I know if I am at risk of developing Peripheral Arterial Disease?
Anyone with Diabetes is at risk of developing PAD, but your risk is greater if you also:
- smoke
- are overweight
- are not physically active
- have high blood pressure
- have abnormal blood cholesterol levels
- have a history of heart disease, or have suffered a heart attack or a stroke
- have a family history of heart disease, heart attacks or strokes
What are the warning signs for Peripheral Arterial Disease?
Many people with Diabetes and PAD do not have any symptoms, while some may experience only mild muscle pain or difficulty walking. Others may experience the following symptoms:
- leg or calf pain or weakness which is worse when walking, exercising or climbing hills, and disappears after a few minutes’ rest
- numbness, tingling or coldness in the feet or lower legs
- sores or infections on your feet or legs that seem to take a long time to heal
- a change in the skin colour of your feet or legs
- hair loss on your feet or legs
- slower growth of your toenails
- no pulse or a weak pulse in your feet or legs
If your PAD is severe, foot and leg pain may even occur at rest, and may even disrupt your sleep. You may also experience temporary relief from pain by hanging your legs over the edge of your bed.
As your PAD progresses, you may develop painful ulcers, most commonly at the toes, heels or sides of your feet. These ulcers can take a long time to heal and may become infected or gangrenous, increasing your risk of lower limb amputation.


How is Peripheral Arterial Disease diagnosed?
To diagnose PAD, your Podiatrist will need to:
- ask you about your medical and family history
- feel the pulses in your feet and legs
- check your skin colour and temperature
- check your ankles for any swelling
- check the growth of your toenails
- ask you about muscle pain in your legs while walking
Your Podiatrist may also apply a test called the ‘ankle-brachial index’ (ABI), which compares the blood pressure at your ankle to the blood pressure at your arm. If the blood pressure at your ankle is lower than the blood pressure at your arm, it indicates that you may have PAD.
Other tests your doctor may use to diagnose PAD include:
- Duplex Ultrasound, which examines both your blood flow and the structure of your blood vessels
- Angiogram, in which dye is injected into your blood vessels and xrays then taken to show whether your arteries are narrowed or blocked
- MRI Angiogram, in which special scanning techniques are used to detect blockages within blood vessels
How is Peripheral Arterial Disease Treated?
Studies have shown walking is the best medicine for PAD, both as treatment and as prevention. The pain caused by PAD, although uncomfortable, is not damaging to your feet and legs, and we encourage you to walk until you feel pain, rest until it subsides, then continue walking, gradually increasing your walking time to 30-60 minutes daily. We also encourage you to take advantage of the Heart Foundation’s free community walking program.
In addition to walking, you can stabilise or improve the symptoms of PAD with the following lifestyle changes:
- quitting smoking – it is a significant contributing factor to PAD. Contact the Queensland Health Quitline for assistance
- lowering your cholesterol – see your doctor, who may prescribe medication if appropriate
- controlling your blood pressure – see your doctor, who may prescribe medication if appropriate
ensuring your blood sugar levels are within a normal range – see your doctor for assistance
If your disability is severe, or your symptoms are deteriorating, you may need a referral to a vascular surgeon, who will assess whether a surgical intervention or endovascular procedure may be necessary. Such interventions might include bypass surgery or angioplasty and stenting.


What should I do if I have Diabetes and Peripheral Arterial Disease?
Foot care is important for anyone with Diabetes, but it is critical if you have Diabetes and PAD. The poor blood circulation caused by PAD can keep any wounds you have from healing and increase your risk of infection, ulceration and ultimately amputation.
The following are simple measures you can take to care for your feet:
- wear well-fitting protective shoes and socks to avoid injuring the skin on your feet
- apply a moisturising cream to your feet and legs daily to prevent dry skin cracks and to help keep your skin healthy
- inspect your feet daily for injuries, and if you notice any cuts, wounds, blisters, malodour, redness or swelling see your Podiatrist as soon as possible to prevent any problems from worsening.
Our podiatrists in Brisbane Northside are experienced in high risk foot care, amputation prevention and diabetes education. Please contact us to arrange an assessment.

