
What are plantar warts?
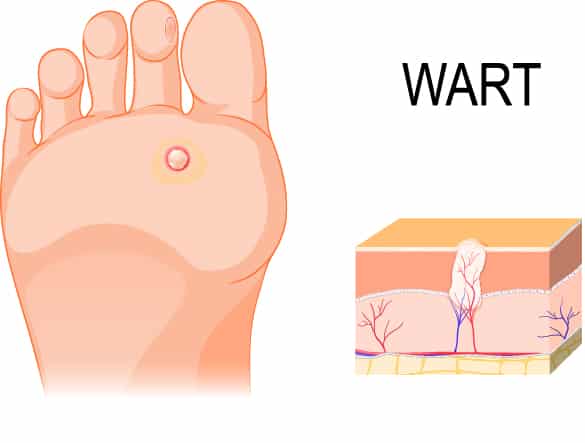
Plantar warts, or verrucae, are benign skin lesions found on the soles of the feet, caused by the Human Papilloma Virus (HPV), which enters your body through tiny cuts, cracks or breaks in your skin.
Plantar warts are rarely a serious health concern, but they may be bothersome, unsightly or painful, and they can also be resistant to treatment.
How are plantar warts different from corns?
Plantar warts are often mistaken for corns or calluses. It is important to make the distinction, however, because the treatment for plantar warts is different from the treatment for corns.
Corns and calluses are caused by increased pressure or skin friction from footwear or abnormal foot posture, whereas plantar warts are caused by direct contact with HPV.


How does HPV lead to plantar warts?
There are more than 100 types of HPV: some tend to cause warts on your hands, fingers or near your fingernails, while others tend to cause warts under your feet.
HPV thrives in warm, moist environments, such as bathroom floors, change room floors and public swimming areas. Infection can be caused by walking barefoot on an infected surface, or by direct contact with skin or blood shed from a plantar wart. If you already have a plantar wart, you can spread the virus to other places on your foot by touching, scratching or picking the wart.
Because each person’s immune system responds differently, not everyone who comes into contact with HPV will go on to develop plantar warts. For reasons not yet fully understood, some people are more susceptible to HPV, just as some people are more likely to catch a cold.
Even people within the same family may react to HPV differently, which is why parents and children will not necessarily spread plantar warts by sharing the same shower. However, children and teenagers tend to be especially vulnerable to plantar warts.
What are the signs and symptoms of a plantar wart?
The most common symptoms of plantar warts are:
- interruption of the normal skin lines, with a ‘cauliflower’ texture to the skin and a well-delineated peripheral border
- pin-point bleeding after removing any overlying callus
- characteristic ‘black dots’ representing clotted capillaries within the wart tissue
- pain or discomfort when the lesion is squeezed from side to side

How are plantar warts diagnosed?
Plantar warts are diagnosed with a clinical history and a close physical examination. Any overlying or surrounding callus will usually need to be debrided so the lesion can be clearly visualised. During debridement, there will often be some pin-prick bleeding, as plantar wart tissue has a good blood supply.
How are plantar warts treated?
Plantar warts are persistent and difficult to treat. No wart treatment works 100 per cent of the time, but we usually recommend the least painful – and least destructive – methods first, especially for children.
To effectively treat plantar warts in children, we first debride the warty tissue with a scalpel, then apply a 60 per cent salicylic acid cream in conjunction with a protective dressing that is to be kept dry and in place until the next appointment. We repeat this process at intervals until the wart is resolved. Most treatments need to be continued for 6-8 weeks (or longer) before resolution.
The salicylic acid cream we use is more highly concentrated than any preparations available at the pharmacy, and needs to be administered with appropriate professional advice and care. It is thought that it works by irritating the wart and surrounding skin, prompting your child’s immune system to recognise the wart as foreign and destroy it.


What happens if plantar warts are left untreated?
Untreated plantar warts can continue to enlarge and spread, developing into clusters called ‘mosaic warts’, and become more resistant to treatment. They may also become deeply embedded within the skin and painful to walk on.
About 40 per cent of people have plantar warts that will disappear spontaneously (without treatment) within two years. However, most people would rather have them treated than wait for them to disappear or perhaps spread.
How can I help my child to avoid developing plantar warts?
You can reduce your child’s risk of contracting plantar warts by encouraging them to:
- Wear thongs in public areas such as swimming pools and change rooms
- Avoid direct contact with warts, including their own
- Not touch or pick at warts, which may spread the virus
Contrary to popular mythology, touching a frog will not give your child plantar warts!


What should I do if my child develops plantar warts?
The best defense against plantar warts is to treat any new warts promptly so that they do not have time to spread.
If you think your child has plantar warts, contact us for diagnosis and treatment as soon as possible.
What if my child’s plantar wart does not respond to conservative treatment?
If your child’s plantar wart does not respond to conservative podiatric care then more aggressive forms of treatment may be considered. These include:
- Freezing (cryotherapy): a common, usually effective treatment, but often considered too painful for young children
- Laser therapy: usually administered by a dermatologist, laser therapy has a good cure rate, but is expensive, painful, carries a risk of scarring and may take longer to heal than other treatments
- Surgical Excision: although once popular, many health professionals now advise against surgical excision of plantar warts because of complications such as painful scarring beneath the foot
- Oral Medication: cimetidine (or tagamet) is an oral medication commonly used to treat patients with gastric reflux or peptic ulcer disease. It is also an immune modulator, stimulating the immune response to the wart virus in children. In warts that are persistent and resistant to treatment, oral cimetidine may be used as an adjunct to topical therapies.


