
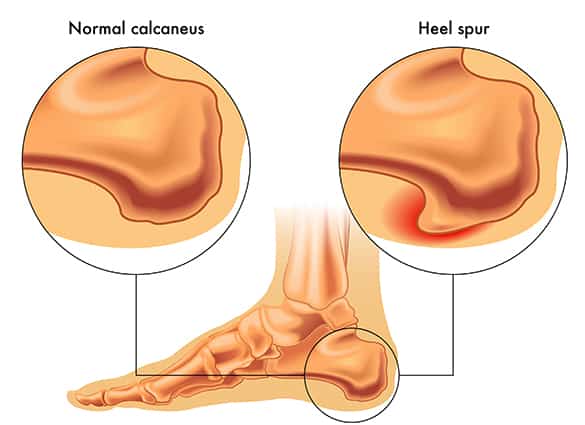
Develops beneath heel bone
A heel spur is a bony protrusion that develops beneath the heel bone. Bony spurs often develop in areas where there is excessive tension, or pulling force, on a bone where soft tissues attach to it. A thick band of soft tissue, called the plantar fascia, attaches to the heel bone and runs across the bottom of the foot to support and stabilize the arch. When there is excessive strain on the plantar fascia, it exerts tension on the attachment site at the heel bone and over time this causes the bone to react by developing a heel spur.
What is the difference between Heel Spurs and Plantar Fasciitis?
Plantar Fasciitis affects the plantar fascia (the thick band of soft tissue that runs along the arch of the foot from the heel to the toes) itself, whereas Heel Spurs occur on the heel bone to which the plantar fasciia attaches. Heel Spurs can develop as a result of chronic Plantar Fasciitis.


What causes Heel Spurs?
Over time, if the plantar fascia continues to pull on the heel bone, eventually a heel spur will form. The plantar fascia exerts excessive tension on the heel bone primarily due to abnormal foot function or foot posture. The same factors that contribute to plantar fasciitis, also contribute to the development of a heel spur. These factors include:
- Abnormal foot posture – if your feet roll in too much (pronate), the soft tissues beneath your feet become overworked and overstretched causing inflammation and pain.
- Muscle Tightness – Tight calf muscles can result in excessive stress being placed on the plantar fascia.
- Unsupportive footwear with poor shock absorption
- Increased Body Weight
- Increased Activity Levels
- Hard Surfaces – walking on hard surfaces (cement or hard-tiled floors) can aggravate heel pain.
What are the signs and symptoms of Heel Spurs?
Many people have heel spurs but may never experience any heel pain and are usually unaware they have a heel spur. In most cases, the heel spur itself is not the cause of the heel pain. The inflamed and injured plantar fascia, or plantar fasciitis, is the most common cause of heel pain. When the heel spur is first forming there may be some bone marrow oedema and this may cause some pain, but once the heel spur has formed this pain resolves. The symptoms of heel spurs are the same as the symptoms of plantar fasciitis:
- Pain in the morning on the first few steps when you get out of bed
- Pain and stiffness (or hobbling) when you start to walk after sitting for a while
- Increasing pain in your heel towards the end of the day
- A ‘bruised’ feeling or dull ache beneath the heel
- Tired feet and legs by the end of the day
- Pain beneath the heel when walking on hard, unforgiving surfaces (eg cement floors or tiles)

How are Heel Spurs diagnosed?
A Heel Spur, or plantar fasciitis, is usually diagnosed after taking a history and performing a physical examination. The physical examination includes:
- testing your muscle strength
- assessing your joint range of motion
- checking your foot posture
- analysing your gait
- testing your ability to perform pain provocation tests
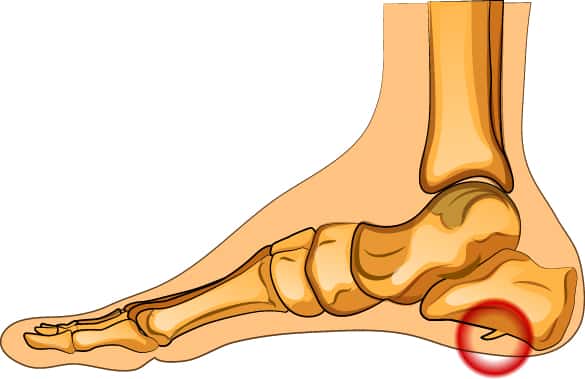
If you have a heel spur this can be seen on a plain foot xray.
Plantar fasciitis can be seen on a soft tissue ultrasound
What should I do if I have heel spurs or heel pain?
You should see your podiatrist as soon as possible if you suspect you have heel spurs or plantar fasciitis.

How are Heel Spurs treated?
Heel pain is the most common complaint of patients attending the Foot Health Clinic and we find that over 90% of the time, it responds well to our treatment program and surgery is almost never required.
Treatment aims to reduce inflammation of the soft tissues that attach to the heel and to improve the alignment and function of your feet. Depending upon the individual contributing factors, treatment may include a combination of the following:
- Rest from aggravating activities and applying ice massage to the heel 3 times daily to reduce inflammation
- Strapping the foot with sports tape can help to reduce excessive strain on the plantar fascia and provide some pain relief
- Orthotic inserts for your shoes – to improve your foot posture and reduce strain on the plantar fascia. Research indicates in cases of mechanically induced heel and arch pain, the most effective treatment is quality custom-made foot orthotics. Orthotics are made from a 3-D scan of your feet and are prescribed specifically to help reduce tension on the plantar fascia and to restore normal joint alignment and function
- Footwear changes – changing to a high quality, stable shoe will help to absorb shock and support and stabilise the foot
- Home Exercise Program – calf muscle and arch stretches are integral to improving foot function and reducing the strain on the plantar fascia. Improving the strength of the foot muscles also helps to support the plantar fascia
- Joint Mobilisation – in addition to a stretching program, joint mobilizations can help to improve flexibility
- Massage Therapy – can be a helpful adjunct to your treatment
- Dry Needling or acupuncture of trigger points in the muscles of the lower leg and foot can assist in reducing pain and improving muscle function and flexibility
- Medication – in some cases a short course of anti-inflammatory medication may also be required to help reduce acute inflammation
- Weight loss if required
The longer heel pain is left untreated, the more difficult it becomes to alleviate with conservative care by your Podiatrist. If heel pain is not treated early cortisone injections, night stretching splints or cast immobilisation may be required.

