
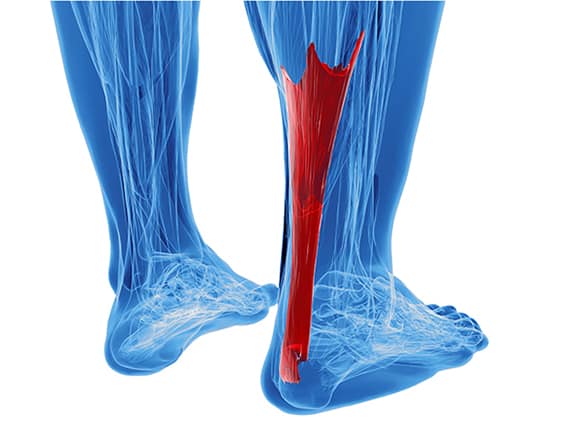
Achilles Tendinopathy
Common among intermittently active
Problems that affect the Achilles tendon are common among active middle-aged people and athletes. Until recently Achilles Tendinopathy was commonly referred to as Achilles Tendonitis. However, research has found that this type of injury does not involve inflammation and is most likely due to a series of microtears (tendinosis) that weaken the tendon.
The achilles tendon is the large tendon located in the back of the leg that inserts into the heel. The Achilles tendon connects the leg muscles to the foot and gives us the ability to push off during walking, running and jumping activities.
Achilles Tendinopathy is most common in people in the 30-50 year age group who are intermittently active.
What causes Achilles Tendinopathy?
There are several factors that can contribute to the development of Achilles tendon problems:
- Change in exercise routine: A sudden increase in the intensity, frequency or duration of exercise activity or a decrease in recovery time between training sessions
- Inadequate warm up, stretching, cool down
- Excessive hill running – this puts the Achilles tendon on maximum stretch
- Wearing unsupportive or incorrect footwear
- Excessive pronation (rolling in) of the foot
- Running or jumping on hard or uneven terrain
- Poor muscle flexibility (e.g. tight calf muscles)
- Decreased joint range of motion (e.g. stiff ankle joint)
- Weak calf muscles
- Overweight, or obese people, are at risk of tendon injuries
- Some medicines (eg. steroids, antibiotics) may increase the risk of Achilles tendon injury

Achilles Tendinopathy
What are the signs and symptoms of Achilles Tendinopathy?
The pain caused by Achilles Tendinopathy can develop gradually and may initially be experienced only after exercise. As the injury worsens pain is often felt during exercise activities and may also be present during normal daily activities. The most common symptoms of Achilles Tendinopathy include:
- Pain and tenderness in the Achilles tendon area, especially if you pinch the tendon between your fingers
- Swelling around the tendon
- Stiffness and pain most noticeable in the morning on first arising
- Weakness when hopping, jumping or skipping on the affected leg
The Achilles tendon can partially tear or completely rupture. While a partial tear presents similar symptoms as a tendinopathy, a complete rupture causes pain and sudden loss of strength and movement. The pain is often described as a hit or kick in the back of the leg.
How is Achilles Tendinopathy diagnosed?
Your Podiatrist will take a comprehensive medical history and perform a physical examination and gait analysis. The assessment will include:
- Foot posture assessment
- Joint range of motion (flexibility)
- Foot and leg muscle strength testing – looking for any muscle imbalance or weakness
- Biomechanical assessment of the foot, ankle and leg
- Footwear assessment
- Gait analysis – to look for any abnormalities in the way the feet move during gait
- Pain provocation tests (tendon palpation, skipping, hopping etc)
- A soft tissue ultrasound scan may also be ordered to look more closely at the tendon


How is Achilles Tendonitis treated?
Conservative treatment for Achilles tendinopathy is most effective when this condition is treated early and may include a combination of the following:
- Rest – from aggravating activities (eg. running, jumping, skipping) until you are able to walk comfortably without pain
- Footwear changes – changing to a high quality, stable shoe will help to absorb shock and support and stabilise the foot
- Orthotic inserts – to improve your foot posture and reduce strain on the Achilles tendon. Custom orthotics are made from a 3-D scan of your feet and are prescribed specifically to restore normal joint alignment and foot function. Non-custom orthotics may also be helpful in some cases.
- Home Exercise Program – exercises to stretch and streng then the Achilles tendon, calf and foot muscles are an integral part of the treatment plan and will reduce the likelihood of injury recurrence.
- Joint Mobilisation – in addition to a stretching program, joint mobilizations can help to improve foot and ankle flexibility.
- Massage Therapy – can be a helpful adjunct to your treatment.
- Medication – sometimes a short course of non-steroidal anti-inflammatory medications (eg. Voltaren, Nurofen) can be a helpful adjunct in reducing inflammation and pain.
- Acupuncture or Dry Needling of trigger points in the muscles of the lower leg and foot can assist in reducing pain and improving muscle function and improving muscle function and flexibility.
- Weight loss if required.
- THOR Low Level Light Laser Therapy
- Foot Mobilisation Technique (FMT)
Return to activity should be gradual and guided by your Podiatrist. A completely ruptured Achilles tendon is most often repaired surgically. Surgery is followed by immobilisation in a plaster cast and then an intense rehabilitation period.
What should I do if I have Achilles tendon pain?
Because of the progressive nature of Achilles Tendinopathy, it’s best to see your Podiatrist as soon as possible. Early treatment of Achilles Tendinopathy has a very good success rate and minimises the risk of a tendon tear or rupture, allowing you to return to your exercise activities sooner. If you think you have Achilles Tendinopathy, contact us.


