Diabetic Foot Ulcers
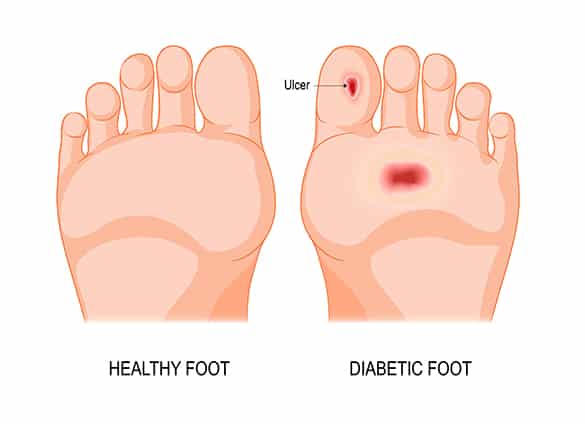
Foot ulcers are sores or wounds on the feet that fail to heal on their own. Approximately 15 per cent of people with diabetes will have a foot ulcer at some time in their lives. Most are the result of injuries that have gone unnoticed, wearing ill-fitting shoes, and walking barefoot.
Foot ulcers are the most common reason for hospital stays, and the most common precursor to amputation, among people with diabetes. Once you have had a diabetic foot ulcer, you are 36 times more likely to develop a foot ulcer or other foot complication in future.
How does diabetes lead to the development of foot ulcers?
There are several factors leading to the development of diabetic foot ulcers:
- diabetes can cause damage to the nerves in your feet, a condition known as peripheral neuropathy, resulting in a loss of sensation and increasing the risk of an injury going unnoticed
- diabetes can cause poor blood circulation in your legs and feet, a condition known as peripheral arterial disease, with the result that any wounds to your feet will take longer to heal
- the elevation of blood sugar levels caused by diabetes can reduce your body’s ability to fight off infection, and delay healing
How do I know if I am at risk of developing a diabetic foot ulcer?
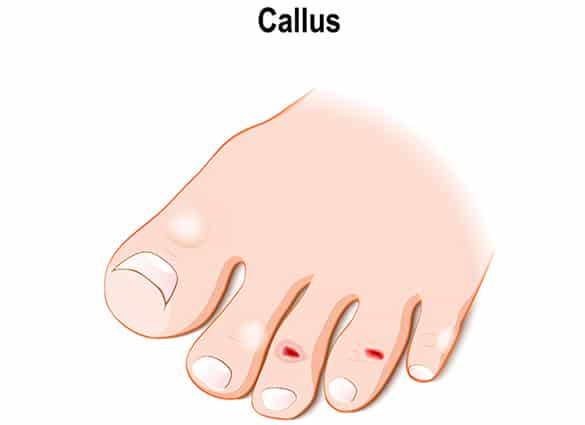
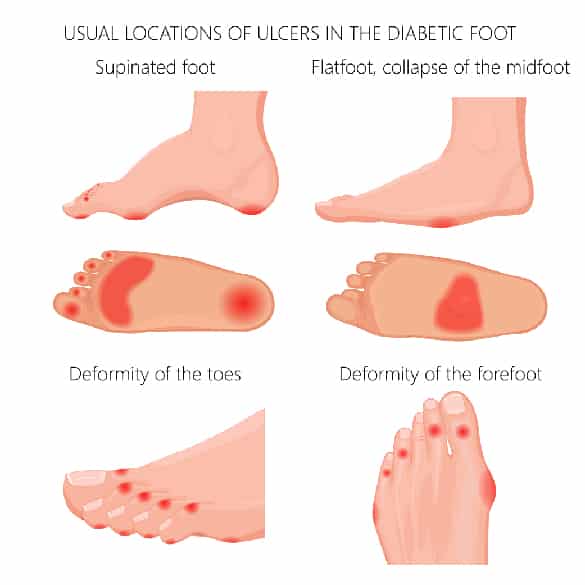
If you have diabetes, you are at risk of developing foot ulcer. The level of your risk increases with the development of diabetic foot complications such as peripheral neuropathy and peripheral arterial disease, and the presence of foot deformities such as callus, bunions, hammer toes and flat feet.
Once you have had a diabetic foot ulcer, you are 36 times more likely to develop a foot ulcer in future.
How are diabetic foot ulcers diagnosed?
Your doctor or podiatrist will conduct examination to determine whether you have a diabetic foot ulcer. Depending on your individual presentation, you may also require tests including:
- a wound swab to check for localised infection
- Radiological imaging – plain xray, ultrasound or MRI scan – to check for soft tissue abscess and bone or joint infections
- Ankle Brachial Index – a test comparing the blood pressure in your arm with the blood pressure at your ankle – to check for circulation problems
- Doppler ultrasound to check any blockages in your leg arteries
- blood tests to check your blood sugar levels, white cell count, inflammatory markers and kidney function
- nerve tests to assess whether you have any loss of sensation in your feet


How are diabetic foot ulcers treated?
Treatment of diabetic foot ulcers may require several steps, including:
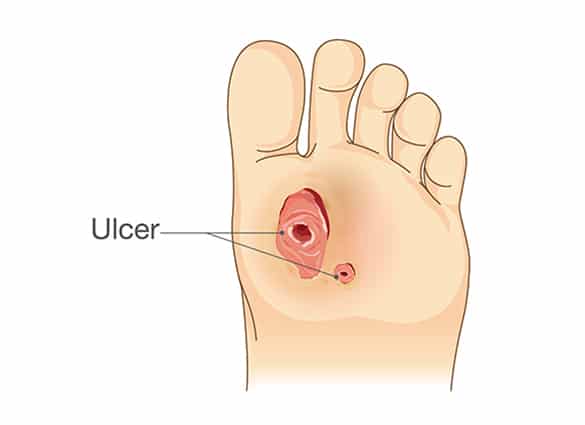
- Taking pressure off your ulcer: most diabetic foot ulcers occur on the weight-bearing surface underneath the foot. For your ulcer to heal, it is important that you do not place weight on the affected area , which may be difficult if you have nerve damage to your foot. Yourpodiatrist will supply you with the most appropriate pressure-relievingdevice (eg plaster cast, removable walking boot, orthotics, brace orhealing shoes) to help you keep the weight off your affected foot.
- Wound debridement: many diabetic foot ulcers have dead tissue and callus surrounding the wound, which need to be removed for optimal healing. Your doctor or podiatrist will perform wound debridement with a scalpel blade or curette, which is unlikely to be painful because of the nerve damage that allowed the ulcer to develop. If there is deep infection in your ulcer, your ulcer will need surgical debridement by a vascular surgeon.
- Wound care and dressings: there are many different types of wound dressings available, and it is important that the right dressing is used to achieve timely healing of your ulcer. Your doctor or podiatrist will select an appropriate dressing depending on the the location of your ulcer, the volume of discharge, the presence of infection, and how often the dressing needs to be replaced.
- Infection control: if your ulcer is infected, your doctor will prescribe antibiotics. A mild, localised infection will require only oral antibiotics are indicated, but a more severe infection may require admission into hospital for the administration of intravenous antibiotics and, if necessary surgery.
- Addressing poor circulation: if you have poor blood circulation in your feet, a vascular surgeon will be consulted to provide an opinion on whether bypass surgery or angioplasty may be necessary to improve the healing potential of your ulcer.
- Controlling blood glucose levels: elevated blood sugar levels impede wound healing, but if your ulcer is infected your blood sugar levels may be difficult to control. Your doctor will advise you on ways to control your blood sugar levels.
- Ensuring adequate nutrition: diabetic foot ulcers place high demand for nutrients on the body and the nutritional requirements for optimal wound healing are generally over and above what is provided by a standard diet. You may need you to increase your intake of protein, zinc and vitamins A and C. You will also need to ensure you maintain adequate hydration, especially if your ulcer is weeping excessively.
How can I help my foot ulcer to heal?
To help your ulcer heal, you should follow your doctor’s and podiatrist’s instructions carefully, paying particular attention to the following:
- stay off your foot – if you continue to walk on your injured foot, your ulcer will not heal, so it is important that your limit all weight bearing activities
- use the wound dressings recommended by your podiatrist and change the dressings as frequently as recommended
- inspect your foot every day for redness, heat, swelling, malodour or increasing discharge, and if you notice any of these changes contact your doctor or podiatrist
- if you have had an infection, ensure you complete your entire antibiotic prescription
- eat a well-balanced, nutritious diet with adequate fluid intake – see your doctor or a dietitian for assistance
- keep your blood sugar levels well controlled – see your doctor for assistance
- quit smoking – if you continue to smoke while you have a diabetic foot ulcer, healing of the ulcer will be significantly delayed. See your doctor or contact the Queensland Health Quitline for assistance
- make sure you attend all appointments with your doctor and podiatrist


How can I prevent diabetic foot ulcers from developing?
If you have diabetes, there are several steps you can take to prevent foot ulcers from developing:
- wear well-fitting, protective shoes and socks to avoid injuring the skin on your feet
- see your podiatrist if you have callus or corns under your feet – callus is a risk factor for ulceration, especially if you have diabetic peripheral neuropathy
- inspect your feet daily for injuries, and if you notice any cuts, wounds,blisters, malodour, redness or swelling see your podiatrist as soon as possible – you may have an infection
- see your podiatrist regularly for a complete foot check-up
Our podiatrists in Brisbane Northside are experienced in high risk foot care, amputation prevention and diabetes education. Please contact us to arrange an assessment.

